Is High Blood Pressure Genetic?

If one of your parents has high blood pressure, you may get it too. Here's how genetics and lifestyle habits may influence your risk.
Is high blood pressure genetic?
High blood pressure can run in families—you might be able to blame it on genetics, as well as similar lifestyle habits.
“When it comes to high blood pressure, the acorn doesn’t fall far from the tree,” says Guy L. Mintz, MD, director of cardiovascular health and lipidology at Northwell Health’s Sandra Atlas Bass Heart Hospital in Manhasset, New York. “If your mom is obese or overweight or has diabetes, you are likely to as well, as these are two high blood pressure risk factors,” he says.
Genes are one part of this, but families also tend to eat the same way and often share similarities in how or if they exercise, Dr. Mintz notes.
Here’s what you need to know about high blood pressure, the potential role of genes in high blood pressure, and available treatment options.
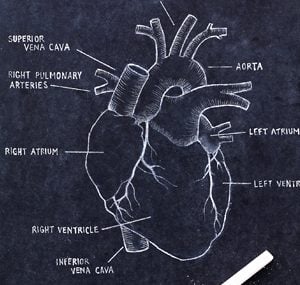
What is high blood pressure?
High blood pressure occurs when the force of blood flowing through your arteries is too strong. Left untreated, it can damage your arteries and lead to heart attack, stroke, kidney disease, and vision problems. It often causes no symptoms until this damage has started, which is why it is known as a silent killer.
Blood pressure is recorded as two numbers. Systolic pressure, the upper number in a reading, is the pressure when your heart beats and pumps blood through your body. Diastolic pressure, the lower number, is the force when your heart is at rest and is filling up with blood. (Here’s how to get the most accurate blood pressure reading.)
A blood pressure of less than 120/80 mm Hg is normal. High blood pressure (aka hypertension) is diagnosed in stages. Stage 1 hypertension is a blood pressure reading of 130/80 mm Hg or higher. Stage 2 hypertension is blood pressure above 140/90 mm Hg.

What causes high blood pressure?
Sometimes high blood pressure is a result of an underlying condition such as kidney disorders, blood vessel disease, or hormonal abnormalities. This is known as secondary hypertension, says Dr. Mintz.
Many things influence blood pressure, including some you can change. These include avoiding unhealthy foods loaded with salt, lack of physical activity, obesity, diabetes, smoking, stress, and consuming excessive amounts of alcohol. Other things—such as age, family history, gender, and race or ethnicity—also affect your risk for developing high blood pressure. However, these risk factors are not in your control. (Get to know these 10 risk factors for heart disease—and how to control them.)
For example, Black people develop high blood pressure more frequently than white people, according to the Centers for Disease Control and Prevention (CDC).
The precise cause of high blood pressure is unknown in as many as 95 percent of cases. This is called essential hypertension. Genes as well as lifestyle factors named above are likely at play, according to the CDC. In fact, more than 100 genetic variations have been associated with essential hypertension.
Blood pressure genes
Some genes may be involved in the renin-angiotensin-aldosterone system, a system that produces the hormones to regulate blood pressure and helps balance fluids and salts in the body. When your kidney can’t properly regulate fluids and salts, blood pressure can rise. Other genes seem to be involved in driving the normal function of the lining of blood vessels.
In a study of blood pressure genes that included 1 million people, researchers identified 535 new gene regions that may influence blood pressure. The study, published in 2018 in Nature Genetics, also found that many of these areas are also involved with the adrenal glands above the kidney and body fat.
To arrive at their findings, researchers cross-referenced genetic information and blood pressure data. Then, they compared the group with the highest genetic risk of high blood pressure to the lowest risk group. They noted that all the genetic variants were associated with having around 13 mm Hg higher blood pressure, 3.34 times the risk of developing hypertension, and 1.52 times the risk of poor cardiovascular outcomes such as heart attack or stroke.
One of the newly discovered gene regions is targeted by an approved type 2 diabetes drug. This suggests that a treatment may already be available if the findings are confirmed, the researchers note. The study also showed that the APOE gene, which is well known for its link to heart disease and Alzheimer’s, also has an effect on blood pressure.
How can I treat high blood pressure?
Currently, there are limited options for treatment until more is known about inherited high blood pressure. Also, there needs to be better matched targeted therapies to reverse or control how the gene affects blood pressure. Lifestyle changes with or without blood-pressure-lowering medication are the way to address high blood pressure and reduce the risk for heart attack, stroke, and other consequences of uncontrolled hypertension, Dr. Mintz says. (Does high blood pressure drugs increase your coronavirus risk?)

Lifestyle changes
“You can’t discount the importance of lifestyle changes when it comes to blood pressure risk,” he says.
Eating a heart-healthy, low-salt diet like the Dietary Approaches to Stop Hypertension (DASH) diet, getting regular physical activity (especially aerobic exercise), drinking alcohol only in moderation, not smoking, and taking steps to change how you deal with stress and stressors, will all make a difference, Dr. Mintz explains.
Certain diets such as DASH—which limits salt, red meat, and added sugar—and the Mediterranean diet—which is rich in fresh fruits and vegetables, lean proteins, whole grains, and healthy fats—are often recommended for lower blood pressure. (These are the healthiest high-fat foods you should be eating more often.)
“Both are great options and fairly easy to comply with,” says Evan Appelbaum, MD, a cardiologist at Men’s Health Boston, a Harvard-affiliated multi-specialty practice. “It’s about finding a healthy way of eating that fits into your lifestyle and you can stick with,” he says.
Exercise
Exercise matters too, he says. Every step you take can help lower your blood pressure, and this adds up to big changes, according to research presented at the 2020 American College of Cardiology’s Annual Scientific Session. In this study, systolic blood pressure was about 0.45 points lower for every 1,000 steps that participants took each day. This means that if you take 10,000 steps a day, you could have a systolic blood pressure that’s 2.25 points lower than if you took 5,000 steps a day. (Here’s how yoga and aerobic exercise can reduce your heart disease risk in half.)
Sleep
Treating sleep apnea, if you have it, can also help reduce blood pressure, Dr. Mintz says.
Marked by pauses in breathing while you sleep, sleep apnea is linked to treatment-resistant hypertension, and it often goes undiagnosed, he explains.
“At nighttime, if your heart is not getting oxygen, it puts out angiotensin II hormones which raise [blood pressure] and cause your arteries to contract,” he continues. Sleep apnea treatment may involve the use of a continuous positive airway pressure (CPAP) device that administers air pressure through your nose while you’re sleeping. (Can’t sleep? Here are 10 possible medical reasons.)
How important is my family history?
In addition to asking about diet, exercise, and other lifestyle habits, your doctor will also ask you about your family history if your blood pressure is high, Dr. Appelbaum says.
“If your parents had high blood pressure or heart disease, we know you are at greater risk, so this guides our treatment decisions,” he says.
“We try to assess cardiovascular risk, and if they or a close family member has diabetes and hypertension, it magnifies things, and we proceed faster with medication than if it’s just hypertension by itself,” Dr. Mintz agrees.
And it turns out that your grandparents’ heart health matters too. A 2017 study in the European Heart Journal suggests that the risk of high blood pressure is not only passed down from parent to child, but also from grandparent to grandchild. Specifically, high blood pressure before age 55 in grandparents was associated with the presence of hypertension in a grandchild. This held even after researchers controlled for other risk factors such as physical activity, salt intake, and alcohol.
What’s more, grandkids rarely lived in the same town as their grandparents, suggesting that they don’t share an environment. This study points to a large role of genes in high blood pressure that still needs to be analyzed.
The last word
Genes aren’t destiny when it comes to high blood pressure. Knowing your numbers and taking steps to get them where they should be are a start. Making lifestyle changes, possibly taking medication, and treating any underlying disorders can help stave off heart attack and stroke.
As researchers understand more about genes and how they increase blood pressure risk, more targeted treatments may be available to aid in these efforts.
Next, here’s how to know when high blood pressure is an emergency.

 Ways to Prevent Heart Disease" width="295" height="295" />
Ways to Prevent Heart Disease" width="295" height="295" />



