
The Highest-Rated Movies on Netflix Canada, According to Rotten Tomatoes
Can't decide what to watch? Start with this list of guaranteed fresh flicks.

Small But Mighty: The Cleanup Kids
How two nine-year-olds started an environmental conservation organization.
Could You Really Be Jailed for Failing to Complete the Census?
If you’re tempted to “forget” to fill out the questionnaire, don’t.

Every James Bond Movie Ranked—From Worst to Best
We review and rank each of 007's globe-trotting adventures from worst to best.

Good News Stories From Around the World That Will Brighten Your Day
The most heartwarming and inspirational good news stories from across the globe.

The Best Thrillers on Netflix Canada You Need to Watch Right Now
From nail-biting murder mysteries to pulse-pounding capers, here are our most suspenseful picks.

Small But Mighty: Cracking the Code
The 18-year-old has been coding since Grade 2. She's now an aerospace cybersecurity expert interning at NASA.

Small But Mighty: 17-Year-Old Saves Soles (and Feet)
18-year-old Indian girl has donated 28,000 shoes over the last five years

Small But Mighty: 17-Year-Old’s Cancer Science Project
Elizabeth Chen data-mined RNA sequences to test effectiveness of cell therapy

Small But Mighty: 15-Year-Old Gallerist Creates Art Opportunities
Nalin Kamat didn't want to see youth shut out of the commercial art world

Small But Mighty: 11-Year-Old Crafts Comforts for Kids With Cancer
Alberta tween with brain cancer enlists some NHL help as a 'childhood cancer awareness warrior'
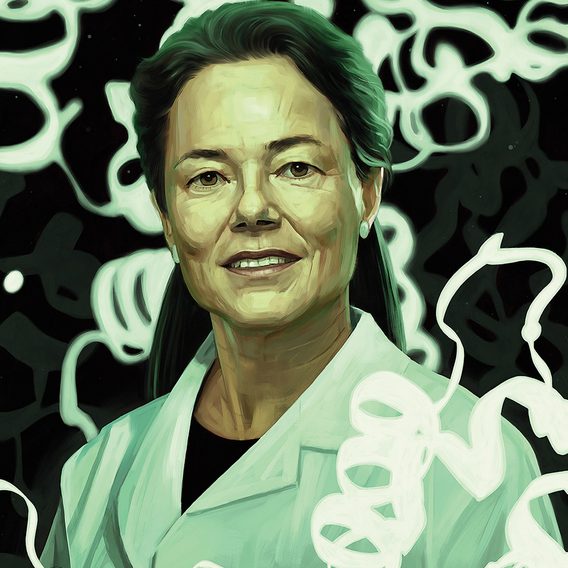
A Mother Was Convicted of Murdering Her Children—Until Science Uncovered the Truth
After all four of Kathleen Folbigg's children died in infancy, a court found her guilty of murder. Twenty years later,...

The Making of Frybread
Frybread, a greasy fried delight made by many Indigenous peoples across North America, tells a story of both resilience and...

Meet the Mechanic Who Modifies Bikes for Injured Veterans
Sharine Milne, an Australian mechanic, customizes bikes so that injured veterans can get riding again.
Hanging Out With Margaret Atwood, Marlon Brando and Pierre Trudeau
In this excerpt from his memoir, Canadian businessman Salah Bachir dishes about the humble private lives of his famous friends:...

Rosie the Dog Got Lost—So She Turned Herself in at a Police Station
After their dog ran off, Steve and Julie Harper barely had time to worry before the phone rang. It was...

After the Family’s Cat Disappeared, a Kind Stranger Reunited Them
A long-haul trucker had an unsuspecting passenger who meant the world to a Saskatchewan family.

As She Rushed to Escape a Wildfire, She Realized Her Dog Was Missing
Yellowknife resident Louise Cumming and her family thought they escaped with all their pets. Until one went missing.

Mushrooms That Could Save Your Food
How mushroom fibre could extend the shelf life of dairy products and even improve wine

Once Incarcerated, This Man Now Helps Youth Lead Meaningful Lives
Ex-prisoner John McAvoy found a new life through sport—and he’s helping disadvantaged youth do the same.

10 Ingenious Innovations That Will Save the World (And Blow Your Mind)
Big thinkers around the world are coming up with ways to make a positive impact. Here are a few of...

13 Magical Facts About Disney Most People Don’t Know
From the making of Mickey Mouse to wild Internet fan theories, these Disney facts are sure to enchant you.

10 Difficult Personality Types—and How to Deal With Them
Got a complainer in your life? Or a contrarian, who always disagrees just for the sake of it? How about...

Unique Ways People are Giving Back Around the World
Charity isn’t only about big donations. Here are the innovative ways people are helping those in need—even when money is...
The Best Books to Gift for the Holidays in 2023
Books make great gifts, but which ones to pick? We’ve rounded up some of 2023’s most talked-about reads.

Best Online Poker Sites Available in Canada Ranked by Traffic & Tournaments (2024 Update)
*All Casinos listed operate outside of Canada with the exception of Spin Casino and JackpotCity, which operate in Canada in...

I Honour My Grandma by Baking Her Christmas Specialty: Cherry Chews
My cherry chews triple the sugar my grandma used. It's the only dish I bake, as a way of honouring...
After Losing My Dad, I’m Learning to Feel the Magic of the Holidays Again
My father had dementia the last time I saw him. But I refuse to let that colour Christmas memories or...

A Canadian Minister Needed a Stem Cell Donor. This Young German Man Stepped In
Dominic Leblanc won seven elections. But he was unlikely to win against non-Hodgkin's lymphoma—until a young overseas donor came to...
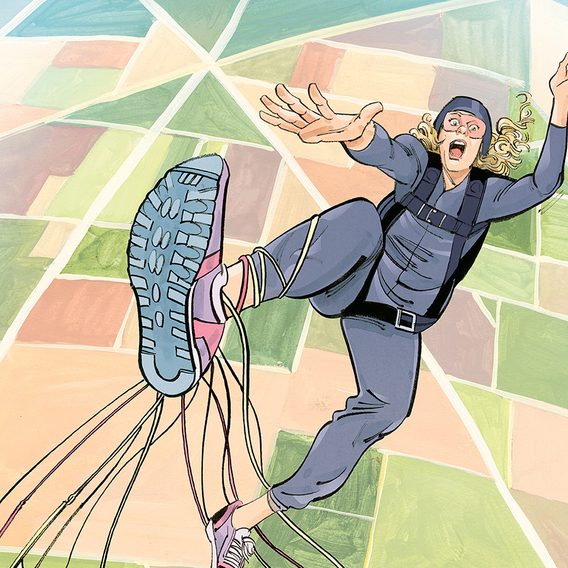
How I Survived A Parachute Malfunction—1,200 Metres Up!
With the ground below her rapidly coming closer and the parachute wrapped around her leg, skydiver Jordan Hatmaker prepared to...

The Architect Who Went From “Starchitect” to Humanitarian
Yasmeen Lari designed gleaming towers for Pakistan’s corporate elite. She now rebuilds villages devastated by natural disasters.